Antibiotic Resistance: An Escalating Global Health Emergency
The rise of bacterial infections that no longer respond to standard antibiotic treatments is rapidly becoming a severe worldwide health concern. Recent global surveillance reveals that antibiotic resistance has increased by more than 40% between 2018 and 2023, with annual growth rates fluctuating between 5% and 15%. This disturbing trend threatens the success of conventional therapies across the globe.
Prevalence of Resistant Bacteria in Common Infections
According to data gathered from over 100 countries through international monitoring systems, nearly one in six confirmed bacterial infections in 2023 showed resistance to at least one antibiotic. These resistant strains are responsible for widespread illnesses affecting millions annually, complicating treatment efforts and increasing healthcare burdens.
Major Resistant Pathogens and Their Clinical Consequences
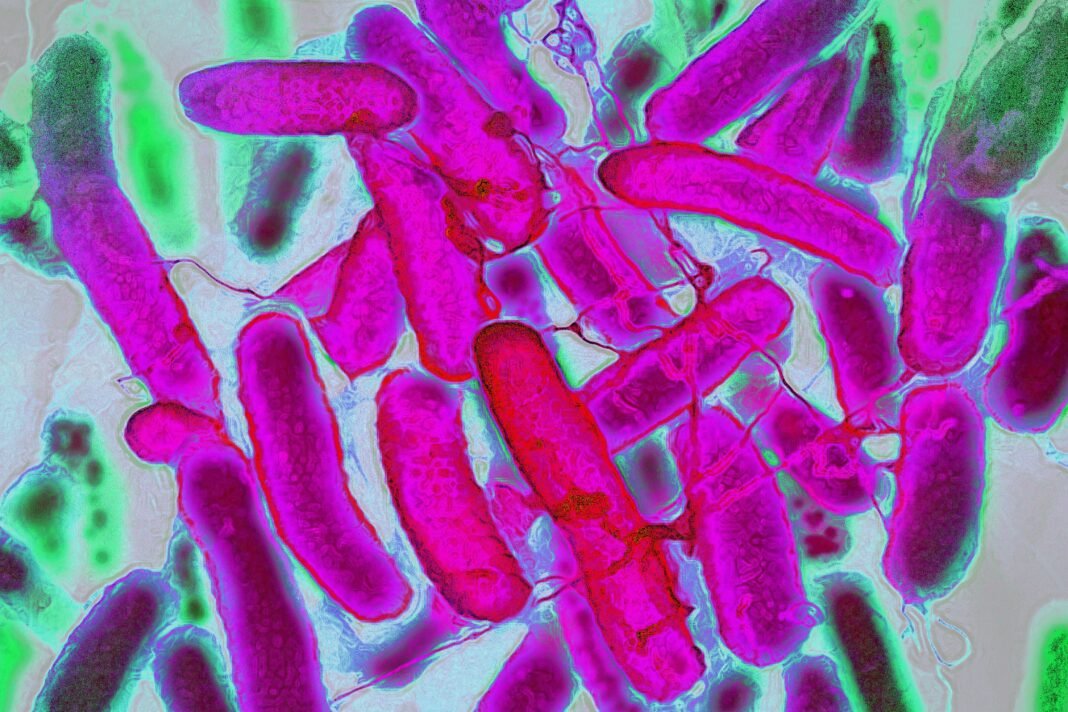
The latest findings focus on resistance patterns against a panel of 22 antibiotics used to treat conditions such as urinary tract infections, gastrointestinal diseases, bloodstream infections, and sexually transmitted infections like gonorrhea. The analysis centers on eight key bacteria: Pseudomonas aeruginosa, Escherichia coli, Klebsiella pneumoniae, Neisseria gonorrhoeae, non-typhoidal Salmonella spp., Shigella spp., Staphylococcus aureus, and Streptococcus pneumoniae.
E. coli and Klebsiella pneumoniae,both gram-negative bacteria,pose some of the greatest threats due to their role in severe bloodstream infections that can lead to sepsis or organ failure. Alarmingly, over 40% of global E. coli isolates now resist third-generation cephalosporins-commonly prescribed frontline antibiotics-while more than half of K. pneumoniae strains exhibit similar resistance levels.

Bacteria such as Salmonella species and Pseudomonas aeruginosa have also developed defenses against critical drugs including carbapenems and fluoroquinolones. This shrinking arsenal forces clinicians to depend increasingly on last-resort medications that are often expensive, less accessible in low-resource settings, or associated with notable adverse effects.
The Widening Divide between Medical Progress and Resistance Growth
The speed at which antimicrobial resistance evolves is outstripping advances in new drug growth as well as infection prevention strategies worldwide. Strengthening antimicrobial stewardship programs-which promote judicious use of antibiotics-and expanding access to accurate diagnostic tools remain crucial steps toward mitigating this threat effectively.
A significant challenge lies within surveillance capabilities; although participation in global monitoring initiatives has grown from just 25 countries in 2016 to over a hundred by early 2024, nearly half failed either to submit data last year or lacked robust systems for precise reporting. Regions like Southeast Asia report up to one-third of bacterial infections exhibiting resistance traits; similarly high prevalence rates appear across parts of Africa where approximately one-fifth demonstrate concerning patterns requiring urgent intervention.
A Unified Global Response Against Antibiotic Resistance
- Improve Data Accuracy: Broaden geographic coverage while ensuring consistent data sharing will enable better tracking across diverse healthcare environments worldwide.
- Cultivate Localized treatment protocols: Customizing national guidelines based on regional antimicrobial susceptibility profiles enhances patient outcomes while reducing unneeded antibiotic exposure.
- Sustain Research Funding: Investing continuously into next-generation antibiotics alongside rapid molecular diagnostics is essential for timely detection and tailored treatment adjustments at point-of-care facilities globally.
- Create Public awareness Campaigns: Educating communities about responsible antibiotic consumption helps curb misuse-a major driver behind rising resistance levels everywhere.
“If left unaddressed, deaths caused annually by drug-resistant pathogens could exceed ten million globally within three decades,” caution health experts highlighting AMR among humanity’s most pressing existential threats.”
Paving the Way forward: Innovations & Preventive Measures
The future depends heavily on building resilient healthcare systems capable not only of preventing infection but also rapidly diagnosing them using advanced technologies such as point-of-care molecular tests deployable even outside sophisticated laboratory settings. Concurrently fostering dedicated research pipelines focused exclusively on novel antimicrobials will replenish dwindling therapeutic options before existing drugs become entirely ineffective due to evolving microbial defense mechanisms worldwide.